
What is Prolapse?
Dr. Marine Lallemant treats patients suffering from prolapse, or organ descent on a daily basis. A condition much more common than we might think… In this article, she talks to us in more detail about this condition- what is prolapse, causes, sypmtoms, prevention and treatment.
What is pelvic organ prolapse?
A prolapse is the result of excessive mobility of one or more organs in the small pelvis. This condition is commonly referred to as ‘pelvic organ prolapse’
Concretely, the pelvic organs in women must have a certain degree of mobility. This is essential to ensure urinary, rectal, digestive, and reproductive functions. Thus, a limitation or, on the contrary, an excess of mobility can be disabling.
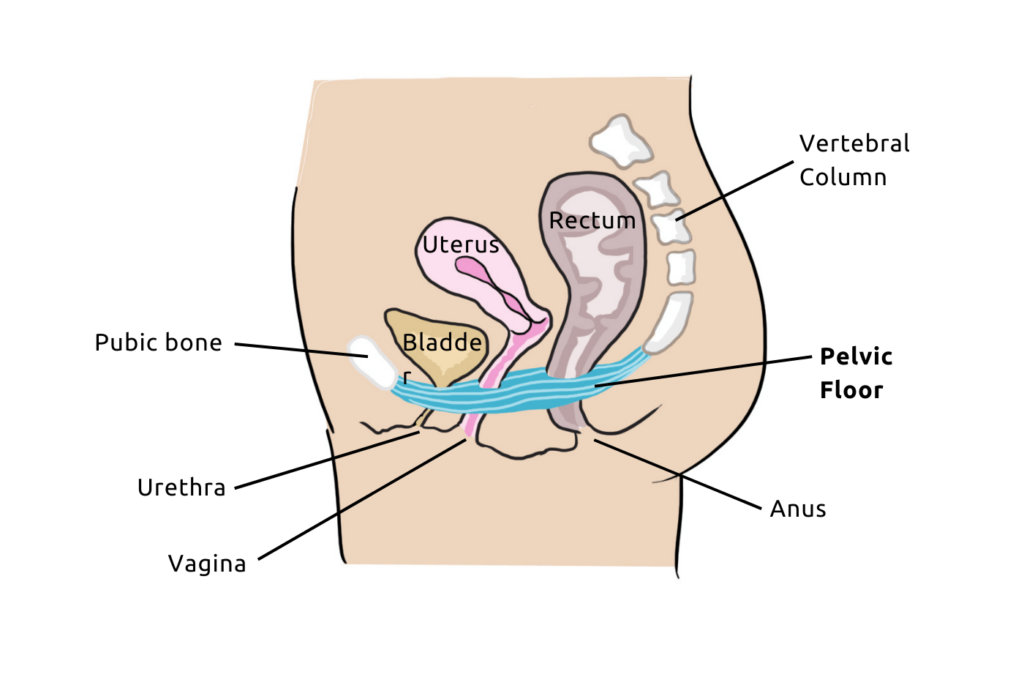
When a woman suffers from prolapse, an organ in her pelvis (bladder, uterus, rectum) slides downwards. In other words, into the vagina.
In the most severe cases of organ descent, it can even protrude beyond the vulva. This is the fourth and final stage of prolapse.
It is also possible that multiple organs descend at the same time. However, it is difficult to assess the frequency of this condition. According to studies, it affects between 4 and 97% of women. The figures vary depending on the method of data collection (questionnaire or clinical examination).
Various types of prolapse in women
There are several forms of prolapse depending on the pelvic organ that descends. These include:
- Cystocele for bladder prolapse: In this case of prolapse, the patient may experience urinary leakage, difficulty urinating, and frequent urinary infections.
- Urethrocele for urethral prolapse: This is the stage preceding cystocele, where only the urinary duct descends into the vagina.
- Hysterocele or hysteropexy for uterine prolapse: The descent of the uterus into the vagina is most often the result of obstetric trauma. It is also possible that the uterine ligaments are too weak.
- Rectocele for rectal prolapse: Anal incontinence (gas and/or stool) may then occur.
- Enterocele if the prolapse affects the intestine: It potentially causes constipation.

How does organ descent occur?
To better understand the process of organ descent, let’s first review the anatomy. In practice, a triple system keeps the pelvic organs in place :
- The pelvic floor muscles (or perineum): Shaped like a hammock, this support system extends from the pubis to the coccyx. The organs of the pelvis (bladder, uterus, rectum) rest on this group of muscles.
- The ligaments: They act as a suspension and anchoring system for the pelvic organs to the bones of the pelvis.
- The fascia: They play a role in the cohesion between the pelvic organs.
Thus, the integrity of this whole system is essential to ensure proper balance. It must be both flexible enough to adapt to pregnancy and childbirth. But also strong enough to resist pressures and even abdominal hyperpressure.

Sometimes, the pelvic floor muscles or ligaments can relax. This relaxation then leads to a descent of organs, which will put pressure on the vaginal wall and deform it. This descent may sometimes go as far as externalizing outside the vagina.
What are the causes of a prolapse?
First, know that the factors favoring organ descent can be modifiable or permanent.
Generally, the triggering and/or aggravating factors are multiple
- Pregnancies, especially when they are multiple and/or repeated.
- Repeated and/or difficult vaginal deliveries.
- Labor with a prolonged duration.
- Difficult delivery with severe perineal tear.
- Median episiotomy.
- High birth weight of the newborn.
- Menopause, which induces relaxation of the muscles and ligaments.
- Surgical operation on a pelvic organ.
- Repeated abdominal hyperpressure: overweight, lifting heavy objects, intense sports activities, constipation, chronic cough, or sedentary lifestyle.
- A disease causing collagen deficiency, a protein essential for the cohesion, support, and strength of tissues. For example, vascular Ehlers-Danlos syndrome.
- Neurological impairments of the pelvic floor (spina bifida, cauda equina syndrome, etc.).
Finally, a woman can develop a prolapse at any time in her life. However, the frequency increases with age, especially after 50 years old. In fact, the risk of surgery for a prolapse after 70 years old is 11%.
Symptoms of prolapse
Now, let’s see what the symptoms of organ descent are. The most common ones are the sensation of a vaginal bulge and the feeling of heaviness.
The patient may also experience urinary symptoms such as urinary incontinence (urine leaks) and pollakiuria (frequent urination). Not to mention urgency (urgent need to urinate) and bladder emptying problems. In this case, she may have difficulty urinating and/or fully emptying her bladder.
Ano-rectal disorders may also occur. For example: constipation, difficulties in evacuating rectal content or anal incontinence (gas or fecal leakage).
Some patients even perform manual maneuvers to urinate or defecate, or to push the organ descent back into the vagina.

Bleeding, pain, urine leaks, vaginal gas during intercourse or loss of sensation… Troubles during sexual intercourse are also possible symptoms.
All these symptoms therefore affect the quality of life of women and impact their daily life (physical or sexual activity, well-being…). They can even become a real functional, psychological, or social handicap.
How to prevent pelvic organ prolapse?
To prevent organ prolapse, it is first necessary to adopt a healthy lifestyle at any age:
- Avoid being overweight by maintaining a balanced diet.
- Adapt physical and sports activities.
- Avoid repeatedly lifting heavy objects.
- Prevent and treat constipation.
- Treat chronic cough and avoid smoking

Furthermore, pregnancy and especially childbirth weaken the pelvic floor. This is why it is necessary to take care of it in the weeks following the birth. The postnatal follow-up appointment (6-8 weeks after childbirth) allows to assess the presence of incontinence or prolapse.
Generally, a gynecologist will then recommend pelvic floor and abdominal postpartum rehabilitation. Regardless of the patient’s condition, these sessions will help her heal or prevent pelvic disorders.

Free Pelvic floor guide
Find out how to strengthen your pelvic floor to prevent bladder weakness and improve intimate pleasure! 💥
I have organ prolapse: what should I do?
To determine if you actually suffer from organ prolapse, a clinical examination is required. A simple examination may be sufficient.
But generally, the healthcare professional will also perform additional tests, such as a pelvic ultrasound or urodynamic assessment. This depends in particular on the type of prolapse and its stage of progression.

Once the diagnosis is official, what can be done to avoid organ prolapse surgery? First, it is necessary to identify the responsible or aggravating factors. Then, conservative treatments are considered to relieve the patient without resorting to surgery.
Firstly, you must follow hygienic and dietary measures. Weight loss, a more balanced diet, and appropriate physical activity (gentle gymnastics, swimming) are good solutions.
It is also important to avoid lifting heavy weights and to treat any problems of constipation or chronic cough.
Then, regardless of your age and the stage of prolapse, the doctor may also suggest the use of a pessary. This is a silicone or latex device to be inserted into the vagina.
By placing it inside, it will help keep the organs in place. Although effective in relieving prolapse symptoms, the pessary does not treat the underlying cause.
Additionally, a local hormonal treatment can be combined with the pessary (local estrogen therapy). This combination notably improves tolerance in cases of vaginal atrophy.
Prolapse and Pelvic Floor Rehabilitation
In addition, healthcare professionals often recommend pelvic floor rehabilitation. The goals are to prevent or slow down the progression of the prolapse. Strengthening the pelvic floor will also help prevent the risk of incontinence.

Furthermore, pelvic floor rehabilitation is very useful after prolapse surgery. This helps promote the recovery of the pelvic floor and prevent recurrence.
Concretely, it involves multifactorial and comprehensive rehabilitation, through contractions and relaxations of the pelvic floor. It improves the tone of the pelvic floor, abdomen, and thoracic diaphragm, as well as the overall lumbopelvic statics.
In addition to sessions with a midwife or physiotherapist, pelvic floor rehabilitation includes self-rehabilitation at home.
In this context, you can use a connected biofeedback device, such as the Emy kegel trainer. It will help you improve your exercises and progress in the right way.

Prolapse Surgery
If conservative treatments are not effective, an operative intervention may be necessary to reposition the organs.
Indeed, surgery is the last resort when organ prolapse reaches an advanced stage and causes debilitating symptoms. In particularly complex cases, a multidisciplinary team of pelvic floor specialists collaborates to decide on the intervention modalities. The choice of the technique depends on various criteria: symptoms, type of prolapse, comorbidities, patient’s expectations, among others.
Of course, surgery will always be associated with managing modifiable risk factors.



