
How to treat vulvo-vaginal infections – bacterial and fungal!
Vaginitis or vulvo vaginal infections are a variety of fairly common pathologies that are often confused with each other. It’s important to distinguish between vaginal bacterial infections and yeast/fungal infections. Intimate disorders that can be particularly bothersome in the daily life of women who suffer from them, especially when this phenomenon has the unfortunate habit of recurring.
What is Vaginitis or vulvo-vaginal infection? The correct diagnosis
Etymologically, the term vulvovaginitis refers to an inflammation of the vulva, and by extension of the vagina. Stated like this, it doesn’t sound pleasant and it’s even less so when we look at the pathologies it concerns: mycoses (fungal/yeast) and vaginoses ( bacterial).

However, fungi and bacteria can each be the cause. Therefore, one should not draw hasty conclusions when symptoms that seem recognizable appear, but rather determine first whether the cause of the infection is bacterial or fungal.
What are the symptoms of vulvo-vaginal infections?
Symptoms of a fungal vaginal infection
In the case of a vaginal yeast infection, specific symptoms are focused on:
- Significant itching in the vulva area, including the labia minora and sometimes the labia majora.
- Vaginal discharge that is more or less abundant, very white and thick,curdled milk.
- The appearance of redness and, occasionally, small bumps on the vulva

Causes of a vulvo-vaginal yeast infection: fungal origin
In the very common case of an infection by the yeast Candida Albicans, the cause may sometimes be found in treatments based on corticosteroids or antibiotics, which weaken the flora.
Urination causes a burning sensation. To be clear about the pathology that concerns us, a gynecological examination with the naked eye is generally sufficient. This examination can be more thorough, thanks to a vaginal swab intended to be cultured in the laboratory.

It is important to note that pregnant women have the particularity of developing candida vulvovaginitis during pregnancy, due to biochemical changes in vaginal secretions, including pH.
Causes and symptoms of Vaginosis- vaginal bacterial infection
Furthermore, in the case of Vaginosis (vaginal bacterial infection) , it is the proliferation of the bacterium Gardnerella vaginalis that is at fault. Impacting one in five women, vaginosis refers to a benign vaginal infection, often recurrent. Its recurrence comes from the cause itself, a flora imbalance is to blame.
Where vaginal bacterial infection confuses things is that, like yeast infections, discharge and irritation are among the symptoms, but to a much lesser extent.
However, the characteristic sign of vaginal bacterial infection that cannot be overlooked is that of fishy-smelling discharge.
Sometimes, there is a discomfort during intercourse and sensitivity of the labia majora. The discomfort and especially the odor are such that it generally dampens the desire for intimacy, yet vaginosis is not sexually transmitted. Having intercourse is therefore possible inspite vaginal bacterial inflamation, provided that desire is present.

Vulvo vaginal infection: treatments
The advantage of distinguishing the type of vulvo-vaginal infection at hand is that an appropriate medical response and treatment can be provided.
Local treatment with a vaginal cream
To relieve a candida-related infection, a cream is applied, systematically combined with an antifungal suppository inserted into the vagina for local treatment.
Natural treatments for vaginitis
Breaking the cycle of recurrence
It can be more difficult to get rid of chronic vaginal bacterial infections. The correct, acidic pH of the flora must be restored by combating situations where blood stagnates in the vagina (heavy and prolonged periods, bleeding between periods) and providing prebiotics that will acidify the vagina again.

Synthetic or too tight and non-breathable outfits also contribute to the development of intimate bacteria.
Stop using sanitary pads!
Furthermore, the excessive use of sanitary pads is not recommended. Stop using panty liners 365 days a year, out of fear of hypothetical vaginal discharge!
If these pads are scented, or if they are made from artificial chemical components that do not meet current standards, this can also harm the flora.

Finally, trying too hard can do harm. Let it be said: vaginal douches are to be avoided.
Pelvic floor rehabilitation sessions
The pelvic floor is the muscular region located between the vulva and the anus. In some cases of recurrant vaginal infections (recurrent itching), pelvic floor rehabilitation can be beneficial.
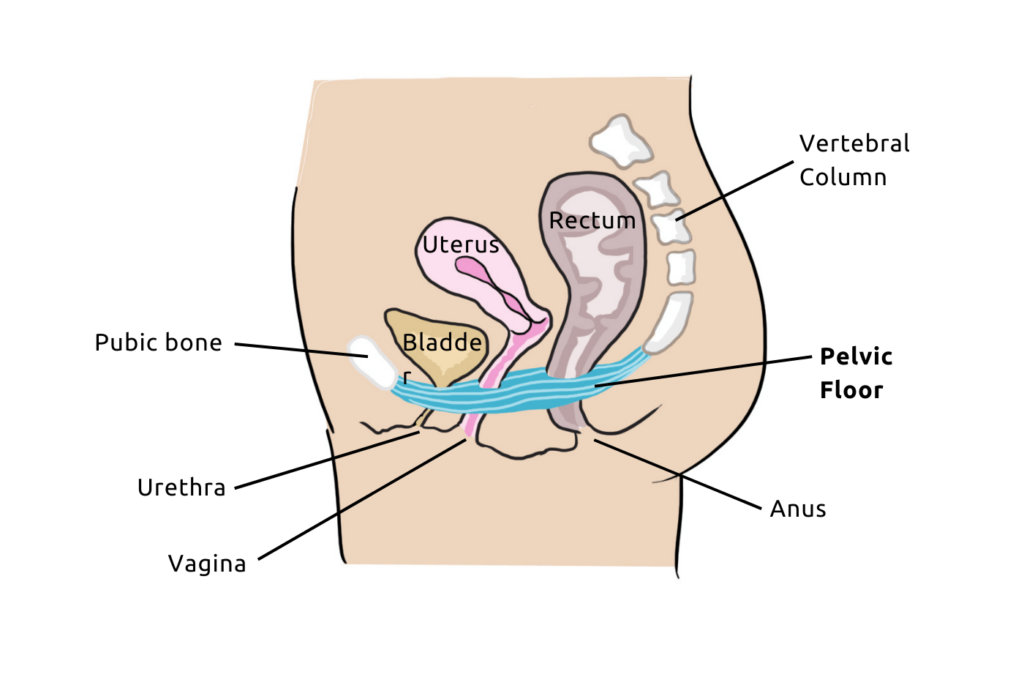
Together with a modification of lifestyle habits, pelvic floor rehabilitation aims to relieve pain and restore tissue flexibility and strengthen pelvic muscles.
So, even though infectionsmainly affects the vulva and vagina, in some cases where there is pain, itching, or involuntary muscle contractions involving the pelvic floor, pelvic floor rehabilitation can be beneficial in addition to other treatments.

Free Pelvic floor guide
Find out how to strengthen your pelvic floor to prevent bladder weakness and improve intimate pleasure! 💥
Vaginitis/Vaginal yeast infection: natural treatments
If you are prone to vaginal yeast infections, know that there are natural methods to prevent and cure them. Here are our top tips.
Coconut oil
Coconut oil is the gentlest natural remedy. It is a natural antifungal that helps reduce inflammation and stimulates the immune system.
Yogurt
It is one of the most common natural remedies. Rich in probiotics, yogurts (organic and natural) are ideal for rebalancing vaginal flora. Consuming yogurt also helps reduce the spread of Candida yeast.
Aloe Vera
Indeed, aloe vera is not just a simple plant! It is a powerful antifungal and natural antibacterial. This is why aloe vera gel can help soothe irritation and relieve inflammation in the affected area.

Here are some simple tips to help prevent vulvovaginitis, which can disrupt your intimacy and cause irritation. However, the key remains to consult a healthcare professional if in doubt, to avoid self-diagnosing incorrectly.


