Pelvic Organ Prolapse Symptoms
We have talked to you about rectocele, cystocele, and pelvic organ prolapse… all these terms may be unknown to some and unfortunately, too familiar to others. Today, in this article, we explain to you what the main symptoms of a pelvic organ prolapse are and its connection with the pelvic floor.
No, this word should not be taboo, quite the contrary. It is important to talk about this condition that affects more than 10% of women at some point in their lives.
How to Detect a Pelvic Organ Prolapse?
A prolapse is the descent of one or more pelvic organs (bladder, uterus, or rectum) into the vagina. These organs, normally located in the pelvic cavity, are held in place by fibers, muscles, or ligaments.
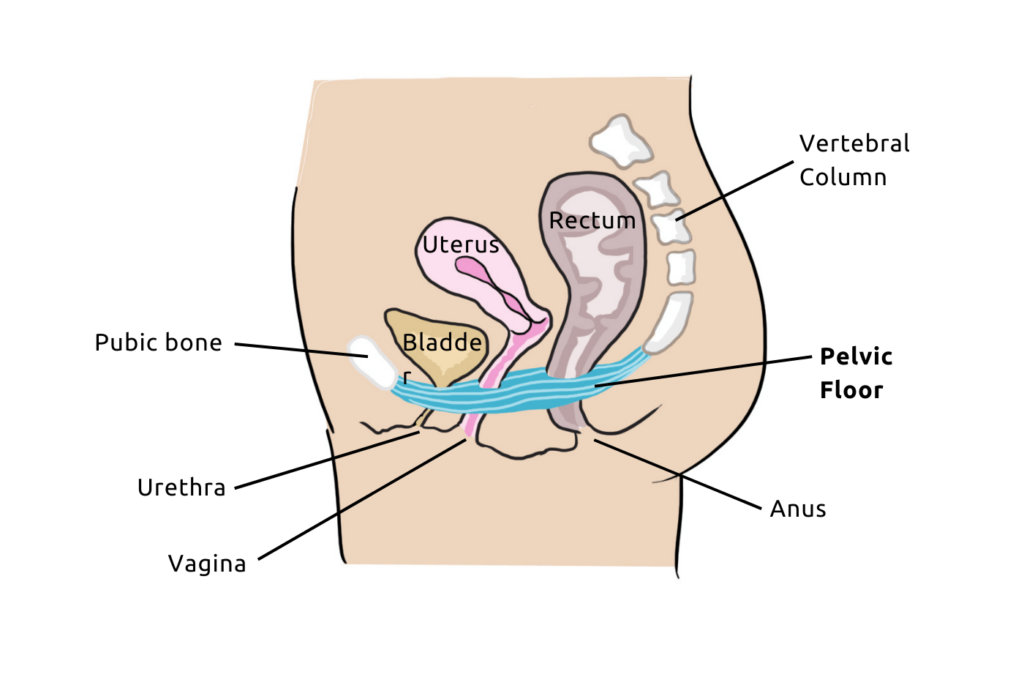
Link between the Pelvic Floor and Pelvic Organ Prolapse
And it is this famous pelvic floor that supports these organs from below (when we told you it was important to maintain this pelvic floor it was not for nothing!). However, the pelvic floor is fragile in women due to the openings that cross the pelvic floor.
Furthermore, it can happen that the muscles and ligaments that support these organs weaken. This can result in pressure on the vaginal wall, sometimes leading to a displacement of a part or all of the organs into the vagina.
Different Types of Prolapse
There are several types of prolapse, but the three main ones are:
- Cystocele (or bladder prolapse): This involves the descent of the bladder into the vagina. It is the most common form of prolapse, occurring in 4 out of 5 cases.
- Hysterocele (or uterine prolapse): This is the descent of the uterus into the vagina.
- Rectocele: As you might have guessed, this is the descent of the rectum into the vagina.
How to Know If You Have a Pelvic Organ Prolapse?
Depending on the stage of your pelvic organ prolapse, certain signs may suggest a prolapse and should alert you. Here are some typical symptoms of pelvic organ prolapse symptoms to watch for.
Symptoms Frequently Associated with Prolapse
When prolapse is not in an advanced stage, it is entirely possible to feel no discomfort. In fact, it is interesting to note that only 10% of women affected by organ descent experience discomfort.

It is therefore important to be very attentive to any other prolapse symptoms that may appear in the lower abdomen region and may be related to organ descent.
For example, the appearance of urinary leaks, urinary infection, anal incontinence, constipation, or if there is discomfort during sexual intercourse, it is important to discuss this with a healthcare professional so that they can establish an overall assessment of the situation and rule out or confirm any associated pathology.
Detecting a low-grade prolapse
Often, discomfort may only occur during physical activity such as sports or lifting heavy objects. If you feel a heaviness sensation in the pelvic floor or vagina, or pressure on your bladder, it is highly recommended to have a gynecological examination by a healthcare professional. It may be a prolapse symptom.
In the case of a cystocele, you may have difficulty urinating (weak stream) and feel like you cannot completely empty your bladder. You may also have a frequent and sudden, irrepressible urge to urinate.
In the case of a rectocele, you may experience difficulty defecating and not be able to completely evacuate your bowels.
Detecting an advanced stage prolapse
When organ descent is in an advanced stage, the genital prolapse will protrude. You may then observe a “bulge” coming out of your vagina. This bulge can cause a feeling of discomfort in the vulva area.
Depending on its location, this may indicate a cystocele if it is located towards the front or a rectocele if it is further back. In any case, the prolapse may worsen if not treated in time. Surgical intervention will then be inevitable.
Factors that worsen organ prolapse
Prolapse can occur at any time in a woman’s life. However, the risk increases with age and tissue relaxation.
Other factors will also increase the risk of prolapse, such as:
- Pregnancy;
- Vaginal delivery;
- Intensive sports activity;
- Overweight;
- Constipation;
- A digestive disorder that requires straining;
- Lifting heavy loads;
- Chronic cough;
- Onset of menopause…

Yes, without you even realizing it, all these factors are intimately linked to the health of your pelvic floor!
Taking care of your perineum throughout your life and strengthening it preventively is essential to avoid organ prolapse. If you are at risk, preventive pelvic floor rehabilitation sessions may be prescribed to you.

Free Pelvic floor guide
Find out how to strengthen your pelvic floor to prevent bladder weakness and improve intimate pleasure! 💥
Strengthening the pelvic floor to prevent prolapse
If you have symptoms or are at the beginning stages of prolapse, perineal rehabilitation is always highly recommended to avoid surgery.
Early treatment of prolapse is not irreversible. Thanks to Pelvic floor training, you can strengthen your pelvic muscles and reduce the risk of worsening your prolapse. However, if the prolapse is at an advanced stage, surgery may still be necessary.
In any case, if after reading this article you suspect you have a prolapse, make an appointment with a healthcare professional who will be able to help and advise you on a suitable treatment.
How to strengthen your pelvic floor?
To strengthen your pelvic floor and maintain a toned pelvic floor, you can visit a healthcare professional (physiotherapist or midwife) to undergo Pelvic floor training
Once these sessions are completed, it is important to continue regularly contracting your pelvic floor to maintain the benefits of the sessions in the long term.

You can continue to strengthen it at home alone thanks to the Emy app, which allows you to perform fun exercises based on medical protocols.
And for an even more effective training, you can use the Emy connected smart kegel trainer to visualize your contractions in real time on your smartphone. This solution allows you to have a real-time follow-up of your progress and improvements.