
How to repair your cystocele?
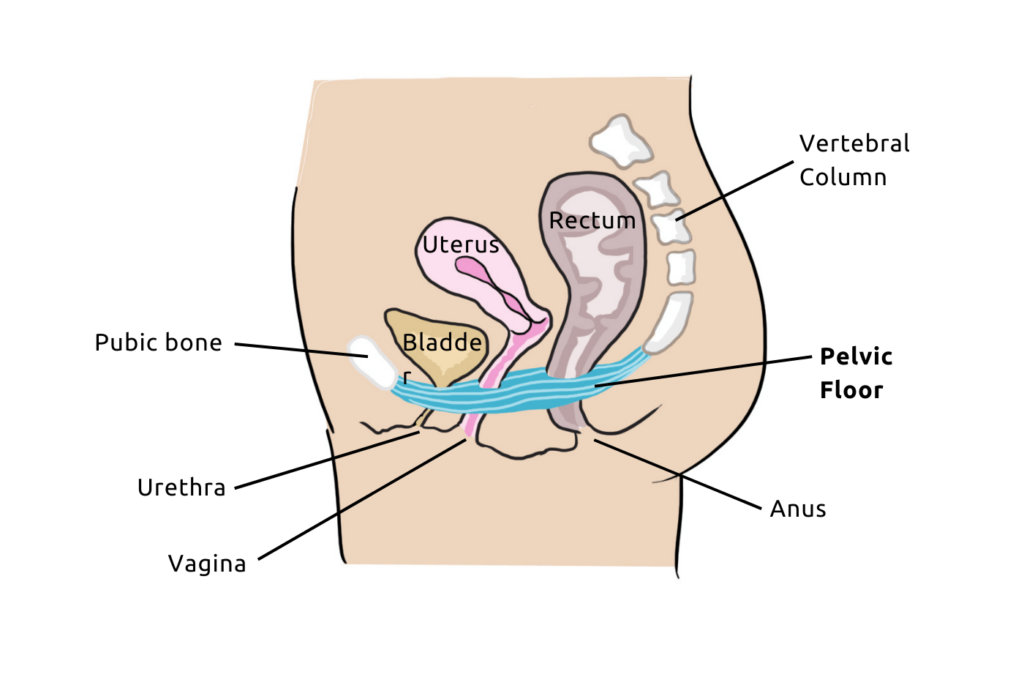
When we talk about the pelvic floor, it is often related to urinary leaks. However, the pelvic floor can suffer from other issues linked to a lack of tone, for example, a prolapse.
Also known as “organ descent“, prolapse can take various forms and is named according to the organ(s) that descends.
The most common prolapse in women is called a cystocele. It corresponds to the descent of the bladder. Let’s focus on the symptoms, causes, and treatments of this condition.

What is a cystocele?
A cystocele is characterized by a descent of the bladder against the vaginal wall. In a cystocele, the bladder leaves its natural position (in front of the vagina, behind the pubic symphysis), to partially descend into the vagina.
The descent of the bladder can continue and protrude if not treated in time. In this case, a lump becomes visible outside the body. Cystocele has 4 severity stages:
- Level 1 -the prolapse is intravaginal and the descent of the rectum is weak
- Level 2- the bladder touches the vulvar orifice without protruding
- Level 3the prolapse extends beyond the vulva
- Level 4 the prolapse is fully exteriorized
What are the symptoms of a cystocele?
A gynecological examination often detects the symptoms of a cystocele. In most cases, women may feel a pelvic or vaginal heaviness sensation. This symptom should alert them and lead them to make an appointment with their healthcare professional.
Generally, urinary issues can be symptomatic of a bladder descent:
- urinary incontinence
- sensation of incomplete emptying of the bladder
- recurring cystitis
- discomfort during sexual intercourse…
What are the causes of a cystocele?
The pelvic floor is one of the main culprits in the occurrence of a cystocele. Repeated pressure on the pelvic floor leads to its weakening. It is no longer able to support the organs under the effect of too much pressure.
All factors that impact the tonicity of the pelvic floor can contribute to the development of a cystocele. For example, these factors may include:
- childbirth
- carrying heavy loads frequently
- high-impact sports activities such as running, tennis, jump rope…
- Obesity
- chronic constipation
- chronic cough (smoking, asthma…)
How to prevent the occurrence of a cystocele?
To reduce the risks, it is possible to implement hygienic and dietary preventive measures. It is possible to easily adjust one’s diet to prevent obesity and constipation. Also, regularly practicing gentle physical activity to protect the pelvic floor can be beneficial.

Regular pelvic floor rehabilitation is also beneficial as it allows to strengthen the muscles of the pelvic floor that support the bladder and genital organs.
How to repair a cystocele?
There are several solutions to treat a bladder prolapse. An appropriate treatment for a patient’s cystocele depends on various factors such as:
- her age
- the grade of the cystocele
- the impact of symptoms on quality of life
- the discomfort experienced…
In all cases, the treatment is adapted to the symptoms and severity of the cystocele.
Initially, a conservative treatment including hygienic and dietary measures (weight loss, combating possible constipation, awareness of overpressure on the pelvic floor, adjusting physical activity, etc.) will be proposed. Additionally, your healthcare professional will also prescribe pelvic floor rehabilitation sessions for you.
Then, the physician may consider treatment with conservative devices (especially pessaries). And as a last resort, they will discuss surgery with you. However, there are also several surgical techniques available. These are to be discussed with the surgeon based on the stage of the cystocele and the patient’s opinion.

Pelvic Floor Rehabilitation to Treat Grades 1 and 2
Pelvic floor rehabilitation is effective for cystocele (and prolapses in general). It focuses on strengthening the muscles that make up the pelvic floor.

Free Pelvic floor guide
Find out how to strengthen your pelvic floor to prevent bladder weakness and improve intimate pleasure! 💥
Therefore, pelvic floor rehabilitation helps counter increases in intra-abdominal pressure and thus fights against cystocele. The muscle work of the pelvic floor also helps to densify the supporting connective tissue, which also improves bladder support.
For this, different forms of pelvic floor rehabilitation are possible. You can go to your physiotherapist or midwife, or if you already know how to correctly contract your pelvic floor.
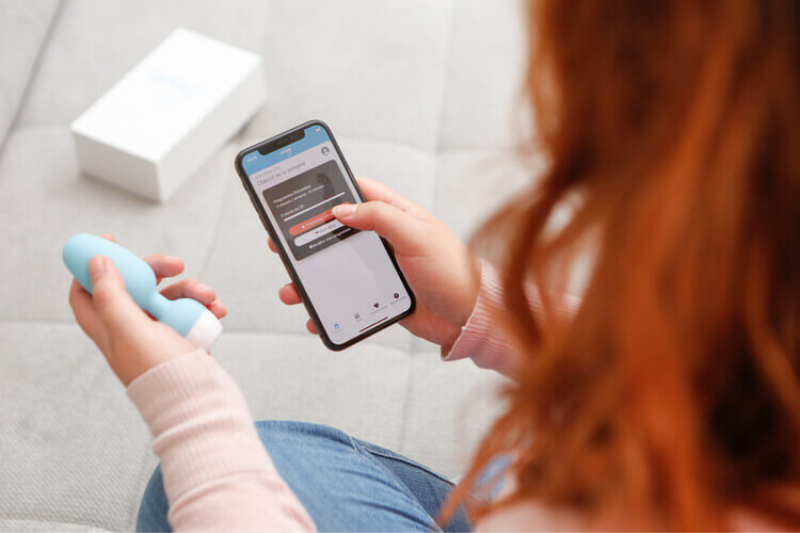
You can also tone it from home with a self-training device. The connected Emy device has, for example, helped Maryse avoid her cystocele symptoms from worsening.
Cystocele repair – Emy smart kegel trainer
The free app “Emy – Pelvic Exercises” offers fun games based on medical protocols and easily accessible from your smartphone. The app helps strengthen your pelvic floor anywhere and, most importantly, at your own pace.

Regularly doing pelvic floor exercises will help maintain this part of your body. Whether to reduce symptoms of cystocele or prevent the development of a prolapse. In any case, by strengthening your pelvic floor and, especially, keeping it toned over time, you will regain control of your body.
Cystocele repair – Using a pessary
Pessaries are small devices that are inserted into the vagina and that help support the bladder. They represent a “mechanical” support solution and can come in different forms: ring, disk, or cube.
Therefore, they are transitional devices. They can be used occasionally during sports activities or worn daily while waiting for surgery, for example.
Cystocele repair- Surgical operation
When cystocele is at an advanced stage, a surgical treatment may be considered. Depending on the patient’s age, the surgeries may vary.
A simpler surgery via lower route (vaginal) will be preferred for older women who no longer have a sexual activity. A more reliable surgery via upper route (abdominal) may be preferred in other cases.
In all cases, we recommend consulting a gynecologist or a urologist. These health professionals will guide you in implementing the most effective solution to address your issue.




